Introduction
Physiotherapy in Redcliffe for Pediatric Issues
Welcome to My Health Teams resource about rotational deformities in children.
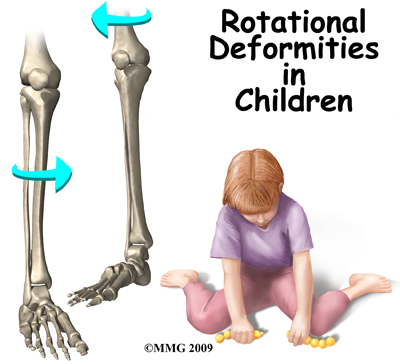
Rotational deformities of the legs and feet in children are often a cause of concern for parents. Most people think of the deformities as either toeing in or toeing out. The deformity actually comes from rotation of the femur and the tibia. Rotation of the legs at birth is normal. Most of the time, the deformities correct themselves by age seven or eight.
Rotational deformities are usually due to position and pressure in the uterus during pregnancy. It is important to determine if the deformity is from this, or from something more serious - like a neurological problem.
This guide will help you understand:
- what parts of the body are affected
- how the condition develops
- how the condition is diagnosed
- what treatment options are available
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Pediatrics|limit:15|heading:Hear from some of our *Pediatrics* patients#
Anatomy
What parts of the body are affected?
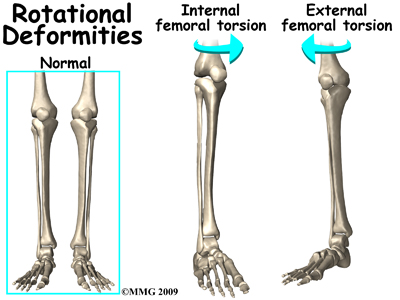
The two main long bones of the leg are the femur and the tibia. The femur is the bone of the upper leg or thigh. The tibia is the larger bone in the lower leg. The front part of the tibia forms the shinbone. The smaller lower leg bone is called the fibula. Excessive rotation (also called torsion) of the femur and/or tibia will cause the foot to appear to either toe in or toe out.
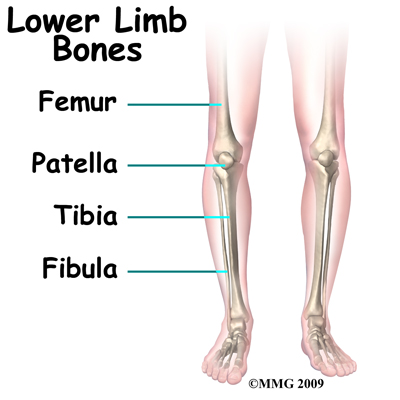
The anatomy of the hip also affects the rotation of the entire leg. The femoral shaft, or thigh bone, attaches to the femoral neck near the hip joint. The femoral neck in turn attaches to the femoral head, the round ball that actually fits into the hip socket. How the femoral neck attaches to the femoral shaft affects how the entire leg lines up with the body.
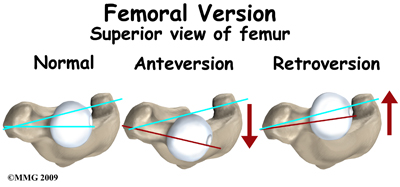
There are two angles between the femoral shaft and the femoral neck that are important. Looking at the front of the body, there is an angle formed where the femoral neck joins the femoral shaft. Looking at the shaft of the femur from the top (along the axis of the femoral shaft), there is also an angle formed between the knee joint and the femoral neck. Doctors call this angle the version of the femoral neck. If the angle is more to the front (anterior) it is called anteversion and if it is more to the back (posterior) it is called retroversion. Normally the version of the hip in the adult is about 15 degrees anteversion.
Version of Femoral Neck
Version can be difficult to understand - even for health care professionals. But remember, the end result is that too much or too little anteversion will make the entire leg look like it is twisted - either the toes turn in or they turn out. Too much femoral anteversion and the toes turn in; too little and they turn out.

Causes
How does this problem develop?
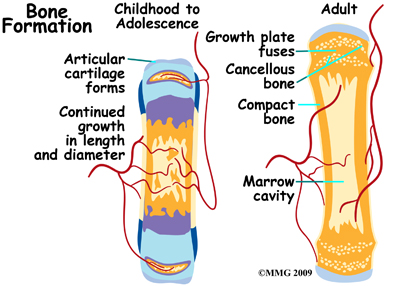
The vast majority of rotational deformities that are seen in children - and worry their parents and grandparents - are normal variations that will improve with time. The infant skeleton is made up of mostly cartilage. It is immature bone. It has not been calcified. This makes it fairly flexible. Babies are packed inside the uterus tightly. Position and compression in the uterus can shape the cartilage. Most fetuses are in a crossed-leg position in the uterus. This affects how our legs look when we are born. Rotation of the legs at birth is not abnormal.
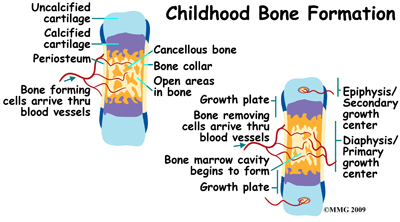
There are usually contractures (tightness of certain soft tissues and ligaments) in the hip and knee joints at birth. This also comes from positioning in the uterus. This can be a part of the cause of these various deformities. Positions for sleeping and play may also help shape the various deformities. Immediately at birth though, changes begin to take place. Throughout childhood, the femur and tibia (and the version of the hip) will continue to change and move towards what is normal for the adult.
Sometimes the rotation at birth is excessive. Five in 10,000 children born will have rotational deformities of the legs. The most common cause is position and pressure in the uterus. An unstretched uterus in a first pregnancy causes greater pressure. This makes the first-born child more prone to rotational deformities. The unborn child grows a lot during the last 10 weeks. The compression or pressure in the uterus increases.
Premature infants have less rotational deformities than full-term infants. This is possibly due to decreased pressure in the uterus. Twins tend to be crowded in the uterus. They are more likely to have rotational deformities.
Sometimes, what is thought to be a rotational deformity is something different. Bowed legs are not necessarily considered a rotational deformity. When rotation is not involved the deformity is called an angular deformity. What looks like bowing of the lower leg can actually be caused by internal rotation of the tibia (lower leg). Because of this, the calf muscles lie on the outside of the leg instead of in the back of the leg. This gives the leg a bowed appearance.
Symptoms
What are the symptoms?
Rotational deformities are most often painless. The exception is with exaggerated femoral internal torsion (or femoral anteversion). Some teenagers and older children with exaggerated femoral internal torsion may develop pain in the front of the knee. Climbing stairs usually aggravates this. Rotational deformities normally do not cause problems in adulthood.
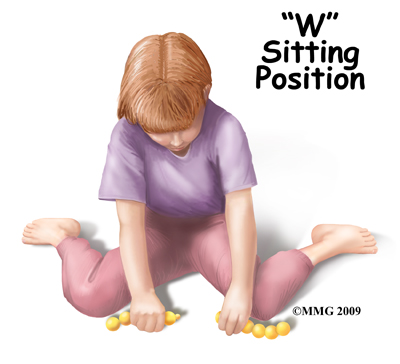
Children with internal femoral torsion may have a habit of sitting in a "W" position, or on their feet, rather than crossed legged. Some children will trip over their feet if they toe in excessively. There is not a delay in the normal development of sitting, crawling, and walking.
"W" Position
 There are four rotational deformities that affect the leg:
There are four rotational deformities that affect the leg:
- Internal tibial torsion (ITT) – causes toeing in
- External tibial torsion (ETT) – causes toeing out
- Internal femoral torsion (IFT) - causes toeing in
- External femoral torsion (EFT) - causes toeing out
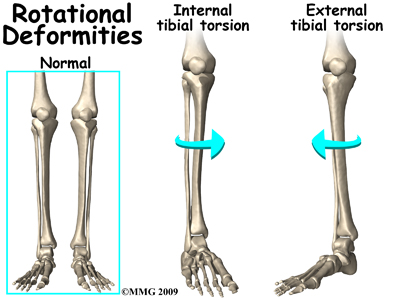
Internal tibial torsion (ITT) is the most common of the rotational deformities. It causes toeing in. It is usually noticed at birth or early infancy. Your child being cross-legged during growth in the uterus causes it. It often goes unnoticed until your child begins walking. The deformity is more obvious when standing. It usually goes away by age two or three. If internal tibial torsion is significant, and lasts past the age of five, surgery to derotate the tibia may be necessary, although this is very rare.
External tibial torsion (ETT) causes toeing out. While the child is in the uterus, the foot is held in extreme dorsiflexion. This means that the top of the foot lies against the shin of the same leg. This causes the foot to be in an externally (outward) rotated position. When your child stands, the foot will appear to toe out.
Internal femoral torsion (IFT) is the most common cause of toeing in after age three. If the tibia and femur are both internally rotated, toeing in may be even worse. This occurs more often in girls than boys. IFT can be diagnosed by comparing internal and external rotation range of motion of the hip. Your child will be placed on their stomach with knees bent. Normal children have equal amounts of internal and external rotation. In children with IFT there is an increase in the amount of internal hip rotation (torsion). Children with internal femoral torsion will want to sit in a "W" position, or on their feet, rather than crossed legged.
External femoral torsion (EFT) is much less common. This is because the usual position in the uterus makes the femur rotate internally, not externally. External femoral torsion can also be a cause of toeing out.
A significant difference between the left and right leg may mean that a deformity is caused by something else. Tumors, abnormal bone formation, fracture, and infection of the bone are possible causes. Excessive toeing out of one foot can be a sign of hip disease. Further evaluation is necessary. A child with progressive bowed legs after 20 months may have a pathological deformity known as Blount’s disease. Rickets can also cause bowed or knocked knees. Rickets is a vitamin D deficiency. It is also seen in kidney problems. Neurological and muscular disorders can also cause deformities of the legs.
Diagnosis
Being that most rotational deformities in children occur without symptoms, it is likely that if you are discussing rotational deformities with your physiotherapist, your child has symptoms that are either a result of the rotational deformities or are aggravated by them. These may include things such as hip or foot pain, and more commonly knee pain. In taking the medical history of the present injury, your physiotherapist therefore may ask many questions regarding your child’s birth. He/she may ask about the pregnancy, labor, and delivery of your child. Your physiotherapist may need to know when the deformity was first noticed. Some are noticed right after birth, others when the child starts to stand or walk, and some are not noticed until after age three. Your physiotherapist will also want to know if the deformity has gotten worse or better over time and if you have noticed an increase in symptoms since the rotational deformity was noticed.
Your physiotherapist will want to examine your child’s legs while your child is in different positions such as standing, or while they are on their stomach with their knees bent. If your child walks, he will want to watch him/her walk. In addition, they will want to feel range of motion of the joints. The legs of the parents may also be examined to see if there is a similar deformity in adulthood.
My Health Team provides services for physiotherapy in Redcliffe.
Our Treatment
Non-surgical Rehabilitation
Most children require no active treatment whatsoever. Generally there are no restrictions placed on young children. Being a child IS the treatment. Allowing the child to pursue normal activity will result in a completely acceptable outcome.
If, however, your child is experiencing symptoms such as hip, ankle, or knee pain, as a result of the rotational deformity, your physiotherapist can help. Commonly older children or teenagers with exaggerated femoral internal torsion may develop pain in the front of the knee.
Initially, the treatment we provide will be focused on pain relief for your child. In the clinic we may use modalities such as ice, heat, or taping and will educate you on the use of these modalities at home as well. Taping the knee can assist in modifying the alignment of the knee joint and kneecap and in doing so, decrease the pain your child feels when walking or being active.
Your physiotherapist is skilled in biomechanical assessment and gait analysis. The next part of your child’s treatment will include an analysis of their alignment and walking pattern. The hip joint is an important controller of knee function therefore this joint will be included in our biomechanical assessment. From this analysis, we will suggest specific individualized exercises for your teen to help strengthen and stretch the muscles around the knee and hip.
Lastly, your physiotherapist at My Health Team will be available to discuss any remaining questions you may have about your child’s condition and, if needed, will refer you onto a Doctor for further discussion.
Post Surgical Rehabilitation
Physiotherapy post-surgically focuses on the same principles as non-surgical treatment. Your physiotherapist will first assist with surgical pain management by applying ice and encouraging gentle range of motion exercises. Once the timing is appropriate, your physiotherapist will assess how your child is using his hip and knee joint post-surgically and also assess their walking pattern. If needed, we will provide the necessary strengthening and stretching exercises to ensure that your child regains the normal use of their leg as quickly as possible.
My Health Team provides services for physiotherapy in Redcliffe.
Physician Review
Your child’s doctor may want to perform a neurological examination as well. This is to make sure there are no symptoms of cerebral palsy, or muscle disease that could be causing the deformity.
The diagnosis of rotational deformity is usually made by the findings of the physical examination. X-rays or other imaging is rarely needed.
If internal tibial torsion (ITT) lasts 18 months after the start of walking, some doctors will suggest the use of a Denis-Browne splint. A bar is attached to the sole of high-top shoes. The splint is worn at bedtime. The feet are forced into a toeing out position.
Your child's doctor may want you to follow up periodically. This is to make sure the skeleton is developing as expected. Most rotational deformities correct themselves by age eight.
Surgery
Surgery is rarely needed to correct the majority of rotational deformities in either the femur or tibia. If external tibial torsion (rotation) is very severe and lasts longer than age four, surgery may be recommended to better align the tibia. Similarly, if surgery on the femur is recommended, it is usually done after the age of eight.
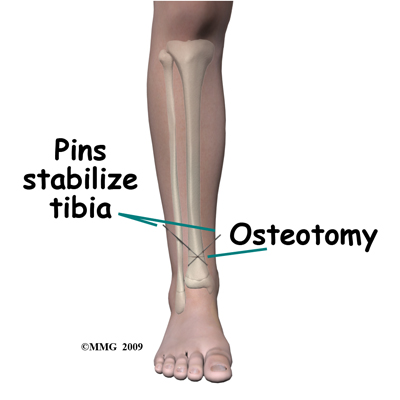
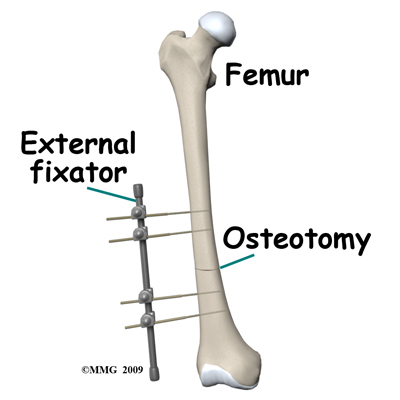
Surgery to correct the deformity is done only when the deformity is severe and affects the child's function. In general, the type of surgery performed to improve the rotational deformity is called a derotational osteotomy. Derotation means to remove the rotation and osteotomy means to cut the bone.
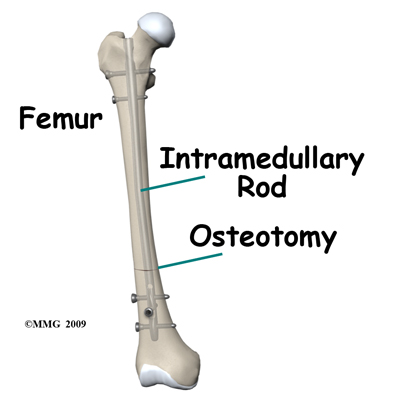
A derotational osteotomy requires the surgeon to cut the bone, rotate it to improve the alignment and hold the bones in that position while they heal. Some type of metal hardware is generally used to hold the bones in place until they heal.
Portions of this document copyright MMG, LLC.
 Get Immediate Access To Your Special Report And Top Tips From Our PTs!
Get Immediate Access To Your Special Report And Top Tips From Our PTs!